More Than Just A Stab In The Dark
MRI Guidance Improves Success & Accuracy of Prostate Biopsy
Prostate cancer is the most common cancer in men in the UK with over 40,000 men diagnosed each year and more than a quarter of a million men living with the condition. Prostate cancer is predominantly a disease of older men (aged 65-79 years) but around 25% of cases occur in men younger than 65 years. Often it can be slow growing and unlikely to have a significant impact on a man’s life. However, a significant proportion of men still suffer with potentially aggressive or life threatening disease.
Currently a man’s risk of having prostate cancer is primarily based on their PSA blood test result and prostate examination. In addition, a strong family history or their ethnic origin may also raise concerns. The only way to definitely diagnose prostate cancer is to have a prostate biopsy where small samples from several areas of the prostate are taken and examined under a microscope. However, there is growing evidence that a detailed functional MRI scan of the prostate prior to a biopsy is important to help localise areas of the prostate that may harbour significant prostate cancer. It is important that these areas when seen are accurately sampled to confirm the diagnosis. The current standard biopsy practice is performed with an ultrasound probe in the back passage with the biopsy needle passing through the rectum into the prostate.
On average about 12 samples are taken randomly from different areas. This test confirms prostate cancer about 35% of the time. The potential downsides of a standard transrectal prostate biopsy are due to the random nature of the sampling and the fact that biopsies are taken via the back passage. Up to one in three biopsy diagnoses of low-volume, low-risk cancers are later upgraded or upstaged. Despite being given antibiotics a proportion of men still suffer from significant infections. Biopsies from the rectum can also miss the front or lower parts of the prostate.
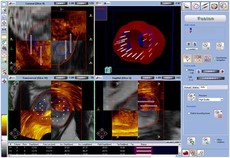
To improve the diagnostic accuracy and also limit the complications, Mr Stephen Gordon has introduced a novel and purpose built MRI and ultrasound fusion device to specifically target suspected cancerous areas of the prostate. In addition, samples can be taken from any part of the prostate and by avoiding the rectum the risk of infection is significantly reduced.
The BiopSee® device fuses the MRI images previously performed with live ultrasound images of the prostate. Any areas of suspicion can then be outlined and specifically targeted in addition to the standard sampling of the different regions of the prostate. The benefit of this approach is that not only is the prostate cancer detection rate likely to be better but that if cancer is found by targeting then it is more likely to be of a significant nature which is best detected at an early stage. Additionally, the transperineal route allows the front part of the prostate, often missed with transrectal biopsies to be adequately sampled and greatly reduces the infection risk. The procedure is performed as a day case under general anaesthetic.
Recently published evidence has shown that an image-guided approach to prostate biopsy is superior for the purpose of detecting prostate cancer especially when the fusion of the MRI and ultrasound images is used. Even more importantly the detection of potentially significant higher grade cancer is also more accurate. This means that for an individual patient, the decisions about treatment options can be more confidently made.
The BiopSee MRI-TRUS Fusion state of the art device provides precise targeting and the best possible prostate biopsy currently available. Whether for a first biopsy or as a repeat biopsy, patients have a greater peace of mind knowing that the chance of detecting significant prostate cancer is maximised whilst minimising the risk of false negative results.
Mr Gordon holds regular clinics at St. Anthony’s Hospital, The Clockhouse Medical Practice and Ashtead Hopsital.
Appointments or enquiries can be made via his PA on 01737 357 258 or by email at enquiries@urology.me.uk.